Home > Clinical Studies > Cryolipolysis for Subcutaneous Fat Layer Reduction
CLINICAL STUDY
CRYOLIPOLYSIS FOR SUBCUTANEOUS FAT LAYER REDUCTION | Avram
Mathew M. Avram, MD, JD1 and Rosemary S. Harry, MSBME2
1Dermatology Laser & Cosmetic Center, Massachusetts General Hospital, Boston, Massachusetts 02114
2 RHarry Consulting, Killingworth, Connecticut 06419
Lasers Surg. Med. 41:703–708, 2009. ! 2009 Wiley-Liss, Inc
Contents
Abstract
Background and Objective: Cryolipolysis is a unique non-invasive method for the selective reduction of fat cells with controlled, localized cooling. It is important, therefore, to understand the potential efficacy and safety of this new procedure for fat layer reduction.
Materials and Methods: A review of the literature associated with cryolipolysis was performed to evaluate the findings from pre-clinical and clinical studies with respect to the mechanism of action, efficacy, and safety.
Results: Cryolipolysis has demonstrated efficacy in both human and animal studies. Histology findings also confirm the selective reduction of fat in both humans and animals, with evidence of a gradual thinning of the fat layer over a period of two to four months. Importantly, cryolipolysis has not produced any significant adverse side effects in studies to date and any noted effects have been minor and temporary.
Conclusion: Although the mechanism of action for cryolipolysis is not yet completely understood, the efficacy and safety of this non-invasive procedure for fat layer reduction has been demonstrated in the studies available to data. Further studies will assist in identifying the mechanism and elucidate the full potential of this technology to perform safe, non-invasive fat reduction for areas of local fat accumulation.
INTRODUCTION
Fat removal and body reshaping, are increasingly popular cosmetic procedures. Currently, liposuction is by far the most common and effective procedure for body contouring. Given the invasive nature of liposuction, and its inherent risks, there has been an ongoing quest for the development of non-invasive forms of body contouring. Various non-invasive techniques have been attempted for body contouring such as laser, ultrasound, radiofrequency, and infrared light, with variable, if any, scientific demonstration of efficacy.
A more recent development in non-invasive lipoplasty has been a novel method of fat layer reduction, termed ‘‘cryolypolysis’’ for the selective destruction of fat cells. This novel non-invasive technology uses controlled cold exposure to effect a gradual reduction of the subcutaneous fat layer using natural thermal diffusion, without damage to other tissues.
BACKGROUND
Numerous studies document that localized inflammation of subcutaneous fat can occur under certain conditions when the tissue is exposed to cold. Such cold-induced inflammation has been described most frequently in infants [1,2], but has also been seen in adults such as females who participate in equestrian activities [3]. Case reports describe the occurrence of a clinically evident inflammation in infants [1,2] as confirmed histologically after apparently minor cold exposure, that is, ice cube application for few minutes. Histological assessment of the exposed areas in some of these infants demonstrated that perivascular infiltration of histiocytes with a few lymphocytes, most intense at the dermal–subdermal junction with extensions into the adjacent dermis and subcutaneous fat, was initiated about 24 hours after cold exposure. The change became more pronounced through 72 hours with the appearance of additional inflammatory cells in the subcutaneous fat, rupture of some of the adipose tissue cells, and aggregation of the lipids. Slight progression of the inflammatory response continued for three more days with histiocytes, neutrophils, lymphocytes, and other mononuclear cells surrounding the adipose tissue cells [1]. Within a few weeks, the cold panniculitis resolved spontaneously without any persistent tissue damage and there was no evidence of cryoglobulins for any of the infants evaluated. Case reports also have been documented of cold panniculitis in women who have been horseback riding in cold and damp conditions [3]. In these women, the inflammatory reaction in the adipose tissue occurred at the dermal– subcutaneous junction with an infiltrate of lymphocytes and neutrophils, as well as a sparse scattering of mast cells and foamy histiocytes. The infiltrate seemed to extend from a perivascular location into adjacent adipose tissue where fat cells were ruptured and small cystic spaces were formed.
PRE-CLINICAL STUDIES
Manstein et al. [4] performed animal experiments to evaluate the potential for selective damage to subcutaneous fat with controlled application of cold to the skin surface. Three complementary pig studies were completed: an initial exploratory study, a dosimetry study, and a safety study to assess the potential impact of such selective damage to subcutaneous fat on lipid levels.
The exploratory study was designed to determine the feasibility of using non-invasive cold exposure to remove subcutaneous fat. A slightly convex, circular copper plate was pressed firmly against the skin surface and cooled by circulating cold antifreeze solution at !78C through a heat exchanger chamber attached to the copper plate. The cold exposure was repeated at multiple sites on the pig, with the exposure time varied between 5 and 21 minutes. The pig was observed for 3.5 months for the appearance and persistence of local fat loss. The amount of fat loss at each test site was estimated relative to adjacent unexposed fat at the margins of the test site.
No apparent skin injury was documented in any of the test areas. There was a slight increase in pigmentation at the 1-week follow-up for some of the test sites but there were no hypopigmentation, scarring, or textural changes. On gross observation, selective fat loss was evident by smooth indentation along the surface of the animal of a size and shape similar to that of the cooling device. A reduction of fat in the superficial fat layer was documented at 3.5 months with 80% of the superficial fat layer removed for a total fat loss of 40% from the procedure. Histology further demonstrated a marked reduction in the distance between fat septae.
The dosimetry study was performed on four pigs with a prototype device (ZeltiqTM Aesthetics, Pleasanton, CA) that contained a thermoelectric cooling (TEC) element. A variable, preset plate temperature was maintained constant during each cold exposure by electronic regulation according to temperature sensors embedded within the cooling plate. Test sites were exposed to either a flat configuration with the device applicator pressed firmly against the skin surface or a folded configuration with the skin fold captured between two cooling plates. The cooling temperature ranged from !1 to !78C for 10 minutes. The animals were sacrificed at selected time points that ranged from immediately to 28 days after exposure. Test sites and surrounding areas were clinically assessed and photographed. Histological analyses of the test sites were also completed using deep tissue vertical sections (skin, fat, underlying muscle) stained with hematoxylin and eosin to assess the level of fat damage as well as potential damage to the dermis or epidermis.
No apparent injury of either the epidermis or dermis was documented for any of the test sites, at any time period, during the dosimetry study. Adipocytes appeared normal immediately and 1 day after exposure, but inflammation of the subcutaneous fat became evident as localized clusters of mixed neutrophil and mononuclear cell inflammatory infiltrate in a predominately lobular pattern became apparent. The inflammation continued to intensify through 30 days following exposure with evidence of phagocytosis. Lipid-laden mononuclear inflammatory cells became abundant, the average size of the adipocytes appeared reduced, and a wider range of adipocytes sizes was apparent. The degree of the inflammatory response was also dependent on the temperature used. Blinded grading of the extent of inflammation of the subcutaneous fat demonstrated that fat damage was significantly greater at lower temperatures and increased significantly over time when compared to an unexposed control.
The lipid level study included six animals for which a relatively large area of the skin surface (15%) was exposed to cooling with a prototype cooling device that included a flat copper plate cooled by a TEC element. Test sites were exposed to temperatures that ranged between !5 and !88C for 10 minutes. Blood samples were obtained after a 12-hour fast prior to treatment, within 1 hour and 1 day, 1 week, and 1, 2, and 3 months post-treatment. The lipid levels over time following cold exposure demonstrated no significant change other than a temporary decrease in serum triglycerides immediately following the cold exposure (attributed to fasting prior to and during general anesthesia).
These pre-clinical animal studies demonstrated that it was possible to non-invasively induce selective, localized damage to subcutaneous fat without epidermal or dermal injury. Selective effects on the subcutaneous fat were evident after exposure to cooling on the skin surface with a range of temperatures and exposure times with both histological assessment and gross observation. Persistent fat reduction without any evidence of damage to the skin or an increase in lipid levels was demonstrated.
The findings from these studies were further supported by additional animal studies performed to assess the ability of cryolipolysis to selectively reduce subcutaneous fat without damage to other tissues or a meaningful change in lipid levels or liver function [5]. Four pigs were treated and survived for 90 days. Three pigs received a single treatment; one pig received multiple treatments staged at 90, 60, 30, 14, 7, and 3 days and immediately prior to euthanasia. Approximately 25–30% of the total body surface area was treated in each animal.
Test sites were exposed to cooling based on the rate of energy extraction, that is milliwatts per centimeter squared (mW/cm2 ). A numerical value, referred to as the ‘‘Cooling Intensity Factor’’ (CIF), was used to express the rate of heat extraction and, therefore, cooling of the skin. The pigs that received a single treatment were exposed to CIF 24.5 (!43.8 mW/cm2 ) for 45 minutes with a 5-minute period of tissue massage. The pig that received multiple treatments was treated with CIF 21.5 (!36.8 mW/cm2 ) for 15 minutes at each site. Treated and adjacent areas were evaluated by standardized flash photography and diagnostic ultrasound after 90 days, and necropsy tissue was collected. Lipid levels were completed (on the single treatment animals) at baseline prior to treatment and at 1 day, 1 week, and 1, 2, and 3 months after treatment.
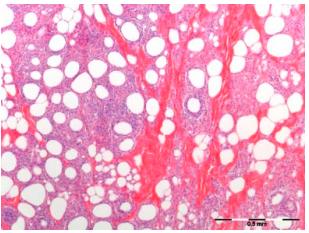
The treatments resulted in a significant reduction in the superficial fat layer without damage to the overlying skin. Smooth inward contour changes, noticeable upon visual examination of the test sites, correlated to decreased thickness of the fat layer as measured by ultrasound 90 days post-treatment. The reduction in the fat layer was 33% as determined from the ultrasound measurements and the pathologic specimens. The reduced fat layer was preceded by an inflammatory response (Fig. 1) triggered by cold-induced apoptosis of adipocytes and subsequent phagocytosis of the lipids. Serum lipids levels remained within the bounds of normal variation throughout the 90-day evaluation period.
Erythema was observed immediately post-treatment and resolved within 30 minutes. The skin was cold to the touch, though not hard or icy, following treatment. There was no evidence of edema, bruising, purpura, or scarring at the time of any follow-up visit or on the day of necropsy. Histologic analysis indicated no discernable damage to the dermis or epidermis in any of the areas treated. In addition, no necrosis was observed in appendageal structures, such as hair follicles or sweat glands.
These animal studies demonstrated that the inflammatory response observed with controlled, selective cooling was consistent with the clinical findings described in the case studies of cold panniculitis observed in infants and female horseback riders. Histological analyses from all of the studies demonstrate that an inflammatory response is initiated in the subcutaneous fat approximately 24 hours after cold exposure. The inflammatory response then continues to intensify with time as the adipocytes are surrounded by histiocytes, neutrophils, lymphocytes, and other mononuclear cells with eventual rupturing of the fat cells.
These animal studies also establish the selective, localized effects of cryolipolysis to significantly reduce subcutaneous fat without causing damage to the overlying skin and the lack of effect on serum lipid levels in the animal model.
MECHANISMS OF ACTION OF CRYOLIPOLYSIS
Histologic analysis at various time periods after cold exposure demonstrates that cryolipolysis results in the death of adipocytes that are subsequently engulfed and digested by macrophages [4,5]. Immediately following treatment, there are no discernible changes in the subcutaneous fat; no inflammatory cells are present and the membranes of the cells are intact. Within 3 days of treatment (Fig. 2A), however, there is evidence that an inflammatory process stimulated by adipocyte apoptosis has begun, as reflected by an influx of inflammatory cells. The inflammation appears to peak at approximately 14 days (Fig. 2B) following treatment as the adipocytes are surrounded by histiocytes, neutrophils, lymphocytes, and other mononuclear cells. Between 14 and 30 days (Fig. 2C) after treatment, phagocytosis of lipids is apparent; macrophages and other phagocytes surround, envelope and digest the contents of dead cells as part of the body’s natural injury recovery response to rid the body of unwanted material. The fat cells become smaller and irregularly shaped as they are slowly digested by the macrophages surrounding them. After this period, the inflammatory response appears to subside and the volume of the fat cells is decreased with apparent thickening of the interlobular septae occurring by 60 days (Fig. 2D). The inflammatory process declines further by 90 days after treatment. The area previously containing fat cells is decreased and the septae constitute a majority of the tissue volume.
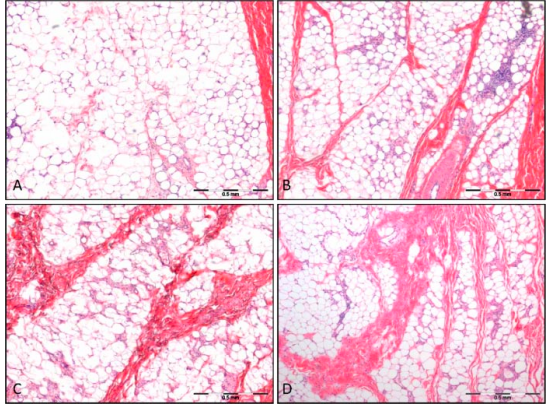
It appears that the lipids remain trapped within the subcutaneous tissue until they are digested and cleared by a natural inflammatory process. This resorption takes place over more than 90 days, resulting in a very gradual displacement of the lipids. The histological results are also visible on gross pathology sections at 90 days, showing a clear reduction in fat layer thickness.
The mechanisms governing the death and subsequent elimination of adipocytes are not completely understood. Initial studies have been performed in an attempt to elucidate a potential pathway [6]. Porcine adipocytes were isolated, cultured and exposed to temperatures ranging from !2 to 288C and 5% CO2 for 1 hour. Following exposure, the cells were returned to normal culture conditions (5% CO2 and 378C) for a recovery period of either 2 or 24 hours. Assays performed to determine the extent of necrotic cell death and apoptotic cell death indicated that adipocytes cooled to !2, 0, and 28C were all necrotically injured regardless of recovery time, as were most of the adipocytes cooled to 78C. Adipocytes cooled to temperatures between 14 and 288C showed no necrotic injury and all showed approximately the same amount of apoptotic injury after 48 hours of recovery. The results at higher temperatures suggest that the mechanism of action responsible for adipocyte death is based on an event that triggers apoptosis although further studies are needed to determine the exact cause of the apoptotic injury.
Thus, the pre-clinical studies confirmed that the phenomenon of cold-induced subcutaneous fat layer reduction could be replicated in experimental animal models. The mechanism for this process, however, remains unclear. Nonetheless, the dissolution of adipocytes in a gradual fashion over a period of months and the consistency of lipid levels following cold exposure suggests a safe process of metabolism.
CLINICAL STUDIES
Cryolipolysis is performed as an outpatient procedure with the Zeltiq System (ZeltiqTM Aesthetics). The device consists of a control unit with an applicator that is applied to the intended area of treatment. Tissue is drawn into the cup-shaped applicator with a moderate vacuum to position the tissue between two cooling panels. The selected heat extraction rate (cooling) is modulated by TEC elements and controlled by sensors that monitor the heat flux out of the tissue.
Once the desired area of treatment is identified, a coupling gel is applied to the skin surface before placement of the applicator to ensure consistent thermal contact. The applicator is positioned on the treatment area with the use of a moderate vacuum. Once affixed on the treatment area, no further operator intervention is required for the duration of the treatment cycle. Treatment with the cold exposure, which includes a predetermined energy extraction rate (CIF, as described earlier) and cycle duration of up to 60 minutes, is initiated. Just prior to the end of the treatment cycle, an electronic pager summons the clinician to be present at the end of treatment, when the system automatically terminates the cold exposure and the applicator is removed from the patient by the operator’s release of the vacuum. Additional applications sites may be treated to ensure that the entire area of desired reduction is appropriately exposed to cooling.
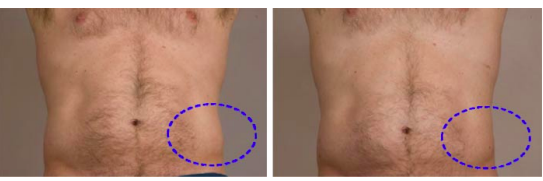
Clinical evaluation of cryolipolysis demonstrates that the selective reduction of fat, as documented in the early animal studies, is replicated in humans. A multi-center, prospective, non-randomized clinical study performed by Dover et al. [7] evaluated the use of cryolipolysis for fat layer reduction of the flanks (love handles) and back (back fat pads). Pre-programmed treatment profiles were used to control the rate of heat extraction and duration of treatment. A contralateral, untreated area was maintained as a control. Based on interim results from 32 subjects, efficacy was assessed by three assessment techniques: ultrasound measurement of fat layer reduction, comparison of pre- and post-treatment photographs, and physician assessment. These assessments confirmed that cryolipolysis results in a visible contour change in a majority of subjects, with the best cosmetic results noted in those patients presenting with modest and discrete fat bulges. Ultrasound measurements taken on a subset of 10 subjects demonstrated a fat layer reduction in 100% of these subjects with an average reduction of 22.4% at 4 months post-treatment. Safety of the cryolipolysis procedure was also demonstrated with these interim results as there were no device-related adverse events reported.
Studies have also been performed to assess whether the cold exposure associated with cryolipolysis is associated with an alteration in local sensory function or nerve fibers, or an elevation in lipid levels or liver functions values. Coleman et al. [8] documented the results of neural assessments and Riopelle et al. [9] assessed lipid levels and liver function tests for 90 days post-treatment.
Ten subjects were treated with a prototype cooling device (ZeltiqTM Aesthetics) during the Coleman study to determine if fat reduction in humans caused by cold exposure is associated with local sensory function or nerve fiber changes. Fat reduction was assessed in 9 of 10 subjects via ultrasound prior to treatment and at follow-up. Sensory function was assessed by neurologist evaluation (n ¼ 9) and nerve staining was completed on tissue obtained with a biopsy from one subject. Treatment resulted in a normalized fat layer reduction of 25.5% at 6 months posttreatment. Transient reduction in sensation occurred in six of the nine subjects assessed by neurologic evaluation. Sensation returned within 7 weeks post-treatment (with a mean of 3.6 weeks). Biopsies also showed no long-term change in nerve fiber structure.
Ten subjects with discrete fat bulges (‘‘love handles’’) were treated with the Zeltiq prototype cooling device during the Riopelle study to determine if a cosmetically significant fat layer reduction was associated with a meaningful change in lipid profile and liver function tests. High frequency ultrasound imaging was used to objectively measure fat layer reduction and photographs were taken pre-treatment and at follow-up visits. Lipid profiles and liver function tests were obtained on all subjects prior to treatment and at baseline, 1, 4, 8, and 12 weeks posttreatment, which ensured that they were assessed through the 90 days after treatment normally associated with peak lipid resorption. Pre-treatment and 6-month post-treatment ultrasound images provided objective evidence of fat layer reduction in eight out of ten subjects. No clinically significant changes or abnormal values were identified for either lipid levels or liver function tests over the 90-day follow-up period.
These clinical studies demonstrate that selective cryolipolysis results in reductions in subcutaneous fat without damage to the surrounding tissues. Ultrasound images and photographic reviews demonstrate fat layer reduction, with the greatest cosmetic improvement observed in subjects with modest fat bulges. See Figure 3. Analysis of lipid levels, neurological response, and the lack of device related adverse events demonstrate the safety of cryolipolysis. Further clinical evaluation is required, however, to more fully understand the potential application to other parts of the body and the optimal treatment parameters for each. Additional studies would also be beneficial to assess whether cryolipolysis poses a unique risk to patients with rare conditions such as cryoglobulinemia, paryoxysmal cold hemoglobinuria, or cold urticaria.
DISCUSSION
Cryolipolysis is a unique non-invasive mechanism for the selective reduction of fat cells. Both human and animal studies confirm previous clinical findings of cold-induced inflammation, as observed in both infants and adults. Histology findings confirm the selective, gradual reduction of fat tissue in both humans and animals. Visual, photographic, and ultrasound evaluations have shown measurable fat layer reduction in clinical studies. Importantly, cryolipolysis has not produced any significant adverse side effects in these studies, no laboratory abnormalities have been noted with lipid levels or liver function values, and any observed effects such as mild discomfort, erythema, bruising, or dysaesthesia have been minor and temporary.
Nonetheless, there are contraindications to cryolipolysis to consider including such cold-induced conditions as cryoglobulinemia, cold urticaria, and paroxysmal cold hemoglobinuria.
Although the mechanism of action for cryolipolysis is not yet completely understood, clinical experience with this device demonstrates that it will be effective for fat layer reduction in confined anatomical areas. At this point, there is no evidence to suggest it can remove fat from large areas on a scale seen with liposuction procedures; however, it is a relatively rapid, non-invasive means of removing localized fat in a safe manner. It requires no pain management, no tumescent or other anesthesia. Moreover, there is no ‘‘downtime’’ associated with this procedure from work or social activities; patients can resume normal activities immediately following the procedure.
Further studies will be needed to more fully characterize the full clinical potential of cryolipolysis and its mechanism of action. Notably, the fat layer reduction provided by cryolipolysis does not approach that of liposuction. Furthermore, it is not a treatment for obesity and patients with significant skin laxity will not appreciate fat layer reduction. Rather, cryolipolysis is best suited for those patients of normal weight with discrete fat bulges. For these patients, cryolipolysis has the potential to provide effective treatment of localized fat accumulation in a safe and gradual manner.
CONCLUSION
Cryolipolysis is a unique method of non-invasive, selective reduction of fat that has demonstrated efficacy for gradual thinning of the fat layer in both animal and human clinical studies. It has the potential to provide safe, effective treatment for the reduction of localized fat in patients with areas of modest fat accumulation. Further studies are needed, however, to assess the full clinical potential of this device.
REFERENCES
- Rotman H. Cold panniculitis in children. Arch Derm 1966; 94:720–721.
- Duncan WC, Freeman RG, Heaton CL. Cold panniculitis. Arch Derm 1966:94:722–724.
- Beachman BE, Cooper PH, Buchanan CS, Weary PE. Equestrian cold panniculitis in women. Arch Derm 1980: 116(9):1025–1027.
- Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowske D, Anderson RR. Selective cryolysis: A novel method of non-invasive fat removal. Lasers Surg Med 2009;40:595– 604.
- Zelickson B, Egbert BM, Preciado J, Allison J, Springer K, Rhoades RW, Manstein D. Cryolipolysis for Noninvasive Fat Cell Destruction: Initial Results from a Pig Model. Dermatol Surg 2009;35:1–9.
- Preciado J, Allison J. The Effect of Cold Exposure on Adipocytes: Examining a Novel Method for the Noninvasive Removal of Fat. Cryobiology 2008;57:327.
- Dover J, Burns J, Coleman S, Fitzpatrick R, Gardner J, Goldberg D, Geronemus R, Kilmer S, Mayoral F, Tanzi E, Weiss R, Zelickson B. A Prospective Clinical Study of Noninvasive Cryolypolysis for Subcutaneous Fat Layer Reduction—Interim Report of Available Subject Data. Laser Surg Med 2009;S21:45.
- Coleman SR, Sachdeva K, Egbert BM, Preciado J, Allison J. Clinical efficacy of noninvasive cryolipolysis and its effects on peripheral nerves. Aesth Plast Surg 2009;33:482–488.
- Riopelle J, Tsai MY, Kovack B. Lipid and Liver Function Effects of the Cryolipolysis Procedure in a Study of Male Love Handle Reduction. Laser Surg Med 2009;S21:82.








